Home-Based Sleep Studies: An alternative to a Sleep Clinic
Various diagnostic testing tests options are used available to determine the presence of Obstructive Sleep Apnoea (OSA). OSA is a common sleep disorder in which numerous breathing pauses occur during sleep.
The main types of tests are Private Home Sleep Studies, Polysomnography (PSG) and Overnight Oximetry. Each type of sleep study requires a sleep recording to assess breathing and oxygen levels throughout the night to help identify sleep–disordered breathing . Your symptoms and medical history will influence the type of test you require, as some as each test provides different levels of detail.
Testing for Sleep Apnoea
In the UK alone, it is an estimated that over three million people suffer from mild to severe Obstructive Sleep Apnoea (OSA) (1). Heavy snoring and daytime fatigue are some of the most common symptoms of OSA.
This fatigue leads to a 6-fold increased risk of road traffic accidents due to poor concentration and falling asleep at the wheel. The significant impact of untreated Sleep Apnoea makes sleep testing crucial for diagnosing the disorder.
Other signs of Obstructive Sleep Apnoea include:
- Memory loss
- Choking in sleep
- Interruptions to sleep
- Poor concentration
- Increased irritability
- Waking up tired
- High blood pressure
- Morning headaches
Types of Sleep Studies
Home Sleep Studies
- Primarily used to detect Obstructive Sleep Apnoea (OSA) events.
- Simple to use from the comfort of your own bed.
- Affordable and less invasive.
- Fast results.
- Clinically validated.
- Suitable for people with symptoms of Sleep Apnoea or other sleep-related breathing issues.
Polysomnography
- Detailed in-lab sleep study used to diagnose a wide range of sleep disorders.
- Overnight test typically completed at a sleep clinic or hospital.
- Typically requires time off work.
- More expensive.
- Waiting list at NHS sleep clinics can be extensive.
Overnight Oximetry
- Monitors blood oxygen and heart rate only.
- Used for one to two nights at home.
- Collection of loaned oximetry machine typically required from sleep clinic or hospital.
- Easy to use but less detailed than other test options.
Why Choose Our Home Sleep Study?

- Free UK delivery.
- Results in two working days.
- Comparable test results to tests done at a sleep clinic.
- Simple to use at your convenience.
- Follow-up clinical consultation included if diagnosed.
- Confidential – we do not inform the DVLA unless you request it, read more on Sleep Apnoea and driving
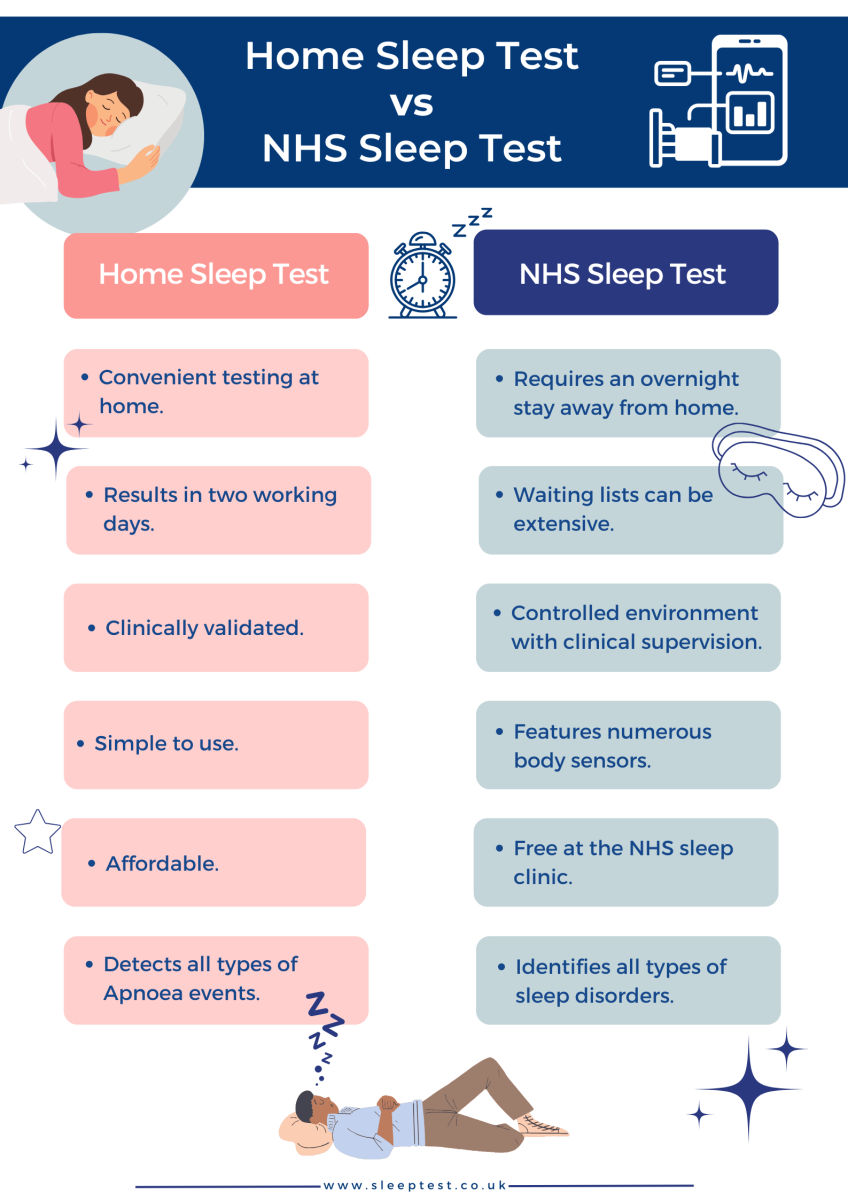
Home Sleep Test vs NHS Sleep Clinic
It is possible to have a sleep test through the NHS with a referral from your GP to an NHS sleep clinic near you. However, it is reported that OSA sufferers in the UK can wait up to two years to receive the treatment they require through the NHS. A report from the BBC in 2020 highlighted this issue.
Read the full article here:- BBC: Up to two-year wait for sleep apnoea treatment
The delay can include waiting for an initial appointment following a GP referral , waiting for the diagnostic sleep test and then waiting again for the results. This can be further compounded by waiting even longer for treatment, including follow-up appointments with a sleep specialist or attending a sleep clinic.
Our test is a great option if you’ve been looking for a private sleep clinic or would prefer not to be on the NHS sleep study waiting list.
If you are experiencing Sleep Apnoea symptoms and are still unsure if you need a Sleep Test, consider taking our free self-assessment risk test. It only takes a minute to complete and assesses your chance of having Sleep Apnoea.
How does a Home Sleep Study work?
Once a test is ordered, it will be sent to you in the post. You will find everything you need to take the test included in your test kit.
Taking the test: You must turn off any transmitting devices (smartwatches, phones, headphones) and remove any tight clothing, jewellery, nail varnish or artificial nails, as these can interfere with the test readings and accuracy.
The WatchPAT device is worn around your wrist. The finger sensor can be placed on any finger (except the thumb) on your non-dominant hand, and the chest sensor should be applied directly to your skin. You can use the hypoallergenic adhesive strips to secure it onto your chest. The test is comfortable and requires one night of sleep data.
Results: One of our sleep specialists will analyse your sleep data and determine whether you have OSA. You will receive a detailed report of the results explaining the data. Results are with you within two working days after completing the test.
Follow-up: Your results letter will state what you should do next. If you have a positive confirmation of OSA, we will advise you of the on appropriate treatment options. We will provide this in your results and guide you through the treatment process.
The benefits of getting tested for Sleep Apnoea
Not only does taking a sleep test lower the risk of developing other health conditions, it can also improve other aspects of your life, these include:
- Better Sleep: OSA disruptions mean you’re not getting the restful sleep you need, which can lead to feeling tired and groggy during the day.
- Safety: OSA can make you excessively tired during the day, increasing the risk of accidents, especially while driving or operating machinery. Testing can help identify if you have Sleep Apnoea and require treatment to stay safe.
- Quality of Life: Treating OSA can improve your quality of life by helping you feel more alert, energetic, and focused during the day.
- Cognitive Function: One of the signs of OSA is memory loss due to the reduced oxygen to the brain during sleep. Treating the condition improves your memory and helps reduce cognitive decline.
- Relationships: Snoring loudly and breathing interruptions at night can disturb your partner’s sleep. Getting tested and treated can help you and your loved ones sleep better.
Polysomnography
If you or your GP thinks you may have Sleep Apnoea, you may be referred to a sleep clinic for a PSG.
A sleep clinic is a healthcare facility that specialises in diagnosing and treating sleep disorders. A PSG is beneficial to those with complex sleep issues, such as those with symptoms of Insomnia, Restless Leg Syndrome, Periodic Limb Movement Disorder, OSA and more. Polysomnography provides detailed information about a person’s sleep patterns and helps diagnose sleep disorders.
Having a PSG test at a sleep clinic will require an overnight stay in an environment that will be different from your usual bedroom setting and will require a different routine in the lead-up to going to sleep. Some people can find this unsettling, causing them to sleep less than they would at home.
For this reason, some prefer to carry out a sleep study at home rather than in a clinical setting.
How does a PSG Work?
Multiple Sensor Placement: During a PSG, numerous sensors are attached to your skin with adhesive to monitor various physiological functions. The sensors monitor eye movements, brain activity, muscle activity, heart rate, chest and abdominal movements, airflow, snoring, leg movements and body positions. A small oximeter is also placed on your finger or ear to monitor your blood oxygen levels.
Monitoring: These sensors collect data throughout the night, and a sleep specialist will monitor your sleep. The specialist will observe your sleep patterns and make any necessary adjustments to the equipment as required.
Follow-up: Once your PSG is complete, the data is analysed, and a report is created. You will be informed of your results and notified of the next steps; this may involve initiating the recommended treatment method.
Polysomnography is a great way to confirm the presence of many different sleep disorders because of its comprehensive monitoring.
A home sleep study is a simpler way to confirm Sleep Apnoea, providing accuracy comparable to Polysomnography in a simplified and portable format.
Overnight Oximetry
Overnight oximetry is a simple test that monitors your oxygen levels and heart rate while you sleep. You wear a small device on your finger called a pulse oximeter. The test identifies drops in oxygen levels, called desaturations, which may signal a sleep-related breathing disorder. This helps identify issues and guide treatment to improve your sleep and respiratory health.
How does Overnight Oximetry Work?
Taking the test: During an Overnight Oximetry test, you can expect to wear the device comfortably on your finger while you sleep. The pulse oximeter will record data and provide valuable information about any fluctuations or abnormalities that occur.
Results: It is a painless and hassle-free procedure that allows healthcare professionals to gather important insights into your respiratory function during sleep. Your results will allow your healthcare provider to evaluate your sleep to understand if you may have a sleep-related breathing disorder.
About Our Editorial Team
Danni is a degree-educated content writer passionate about helping those with Sleep Apnoea sleep better; she works closely with our clinical and customer care teams to ensure that each article is thoroughly researched and accurate.
Her writing aims to inform, support, and advise readers about Sleep Apnoea, helping to raise awareness and promote effective treatment options.
She has written many health-focused articles, reaching hundreds of readers annually, to help people sleep better and live healthier lives.
Lateisha King is an experienced Sleep Clinician with advanced training in polysomnography and respiratory health.
With over six years of experience, including at the prestigious Guy’s and St Thomas’ NHS Foundation Trust Hospital, she has conducted and reviewed more than 500 diagnostic sleep studies.
Her expertise in sleep science ensures that all articles align with the latest data and treatment protocols, providing readers with trustworthy and practical advice to improve their sleep health and overall well-being.
References:
- British Lung Foundation. (2015). Obstructive Sleep Apnoea ToolKit. Available at: https://www.asthmaandlung.org.uk/sites/default/files/OSA_Toolkit_2015_BLF_0.pdf. 16.01.2024


