How to Know if You Have Sleep Apnoea

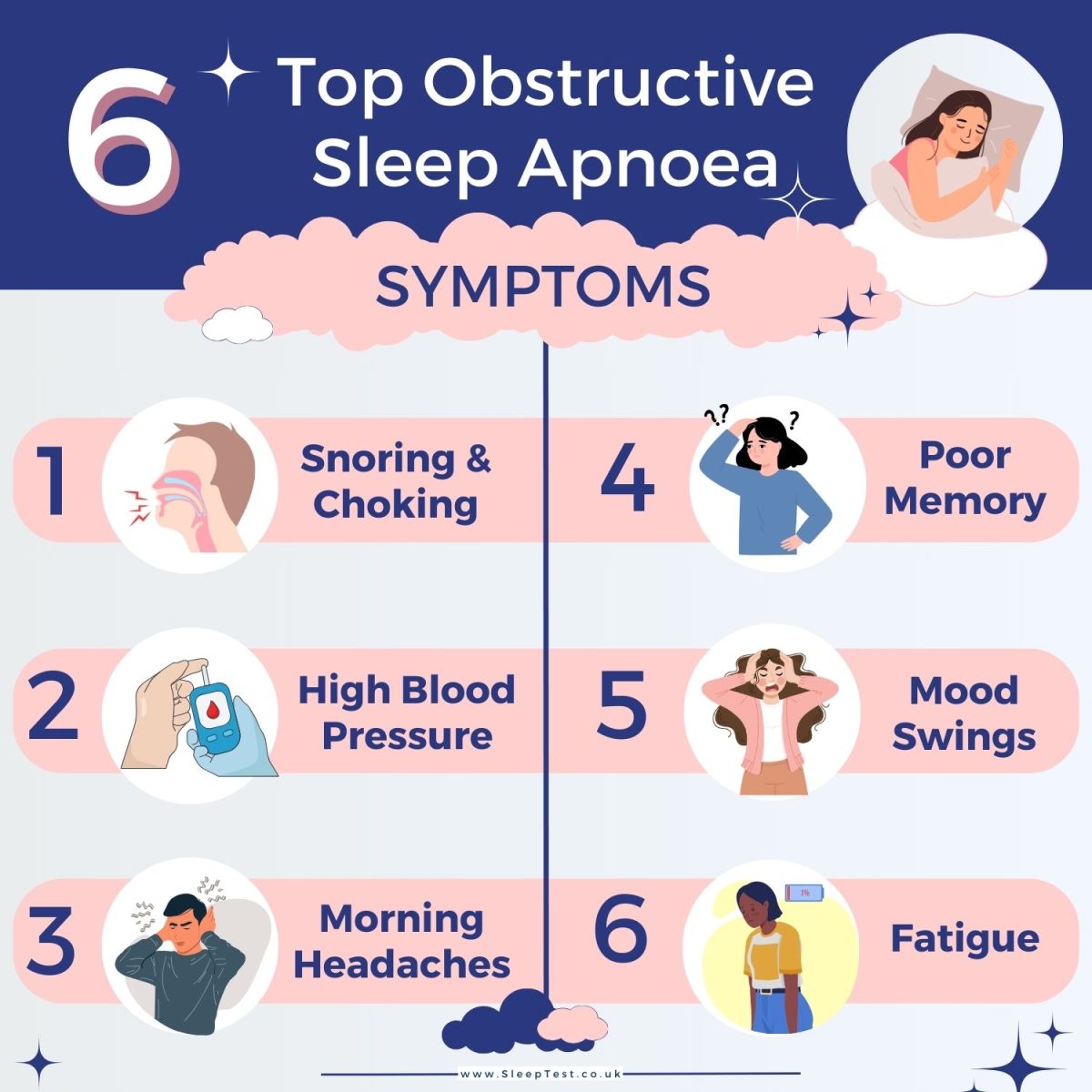
What is Obstructive Sleep Apnoea?
Obstructive Sleep Apnoea (OSA) is the most common type of Sleep Apnoea and occurs when the airway is partially or completely blocked during sleep. This causes continuous breathing pauses during sleep, which can last from a few seconds to minutes throughout the night. These breathing interruptions disrupt the sleep cycle, leading to fragmented sleep.
Sleep Apnoea is a common sleep disorder that affects millions of people in the UK. It can cause the development of various other health complications and affects quality of life.
Getting a Sleep Apnoea Diagnosis
The second step of diagnosing Sleep Apnoea is to confirm your diagnosis with a sleep test. If you have suspected OSA, our home sleep test is a quick and affordable way to effectively detect and diagnose Sleep Apnoea at home.
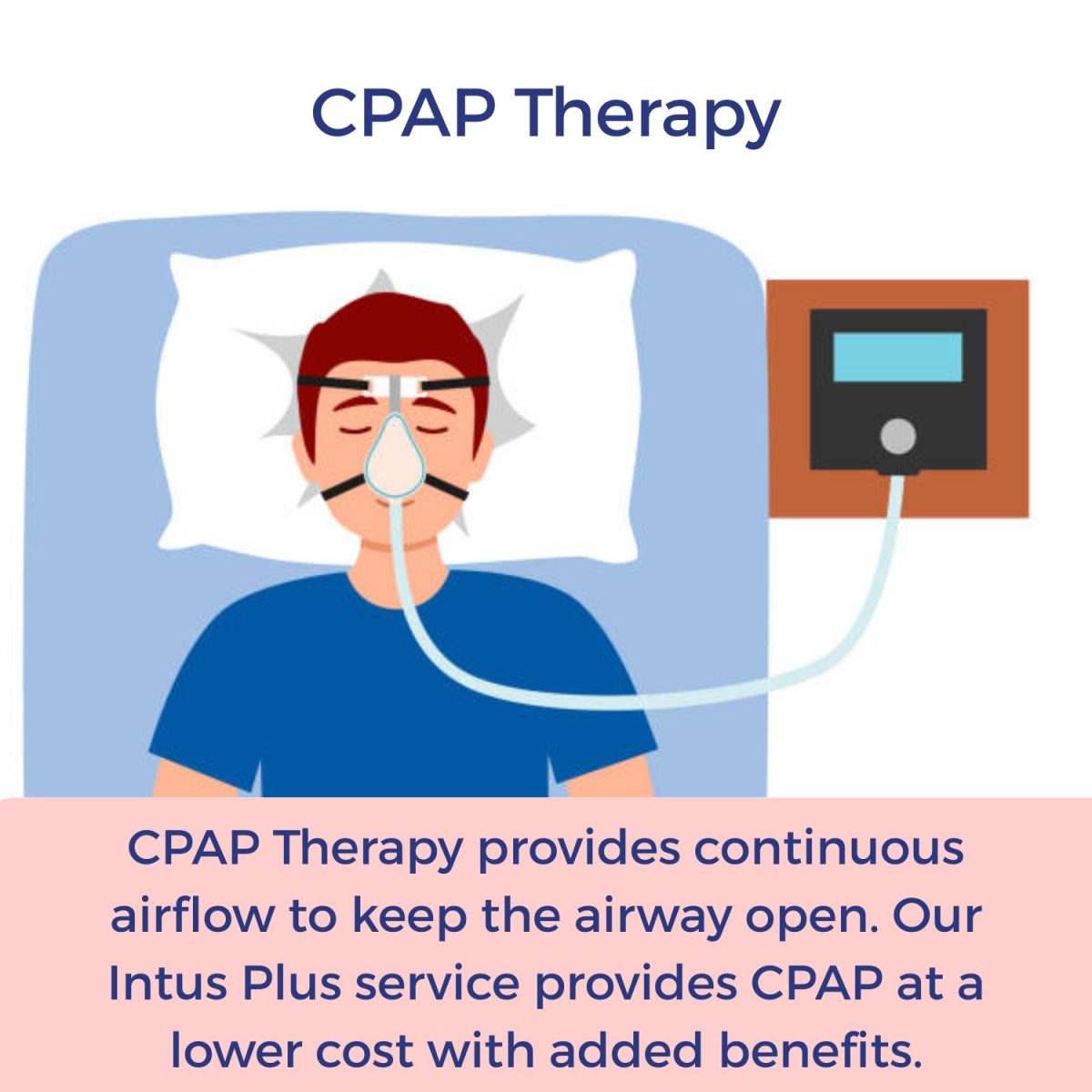
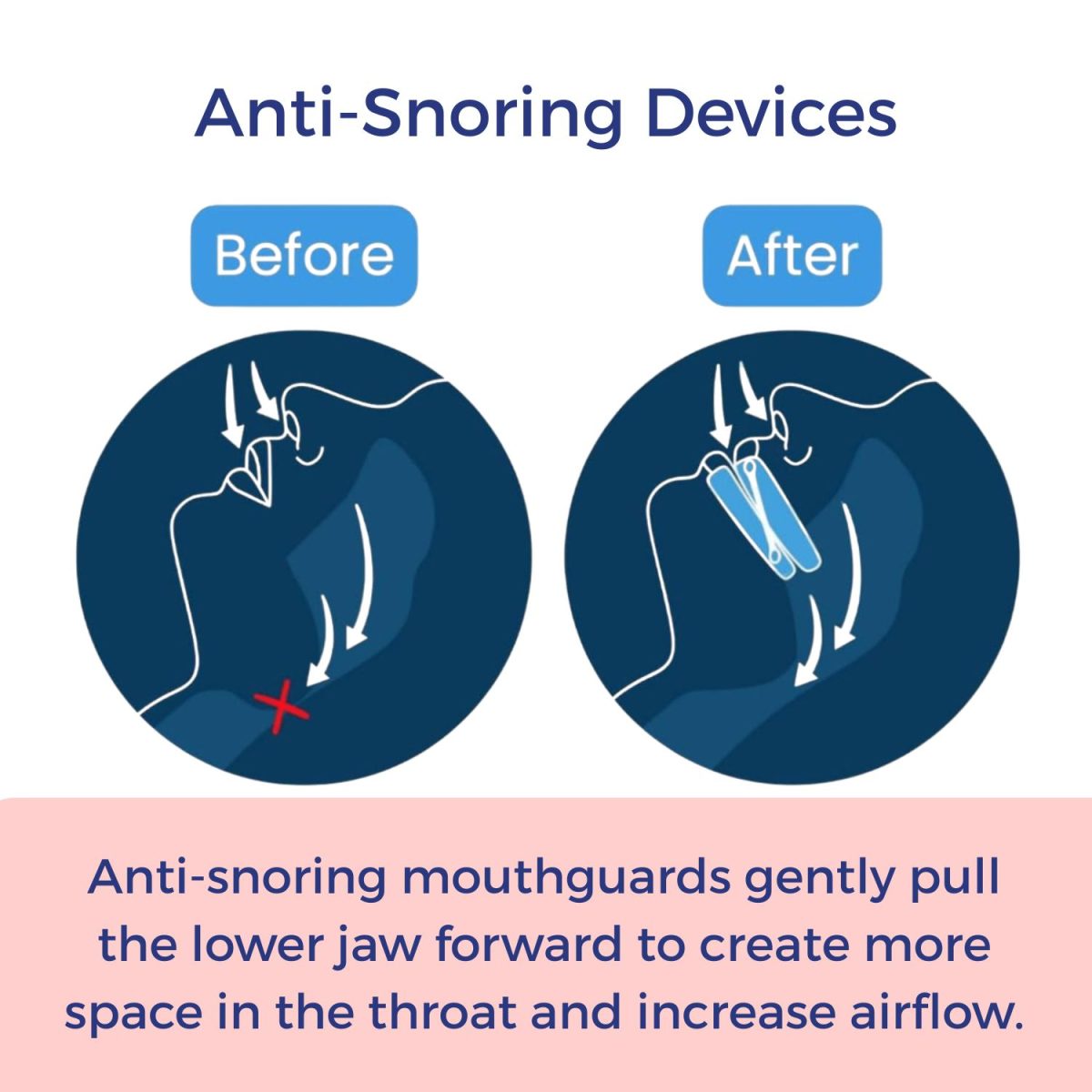
Starting Treatment
Once Sleep Apnoea is diagnosed with an OSA test investigation treatment can start. There are various home treatment options that are dependent on the type and severity of a persons snoring and Sleep Apnoea.
Unsure whether to order a sleep test? Take our free Sleep Apnoea risk quiz

