Sleep Apnoea Symptoms, Causes and Treatment
Sleep Apnoea is a common sleep disorder, affecting millions worldwide, it causes breathing to stop and start repeatedly during sleep. These breathing interruptions reduce airflow and blood oxygen levels, which can leader to significant effects on overall health and sleep quality. This article will explain the types of Sleep Apnoea, common symptoms, and how to diagnose it.
Types of Sleep Apnoea
There are three types of Sleep Apnoea:
Obstructive Sleep Apnoea
Obstructive Sleep Apnoea (OSA) is the most common form of Sleep Apnoea, caused by blockages in the upper airway during sleep. Studies have shown a significant increase in the prevalence of OSA over time, with 22% of men and 17% of women reported to have the condition (1).
These blockages are primarily caused by the relaxation of soft tissue in the mouth and throat which lead to airway obstructions. This causes shallow breathing and breathing pauses reducing the amount of oxygen reaching the body. In response, the brain briefly arouses the sleeper to reopen the airway, often causing sudden moments of waking, gasping, or choking, typically without the person being aware.
Central Sleep Apnoea
Central Sleep Apnoea (CSA) is differs from OSA, as it occurs when your brain doesn’t send the correct signals to the muscles that control your breathing. This means your body forgets to breathe for short periods while you’re asleep. This condition is less common than OSA but can result in similar symptoms such as disrupted sleep and feeling tired during the day.
Complex Sleep Apnoea
Complex Sleep Apnoea is a combination of OSA and CSA and is far less common. Its also known as treatment-emergent central apnoea as it is developed when someone with OSA starts treating the condition with CPAP or BiPAP therapy. Because of this, managing patients with complex Sleep Apnoea can be more difficult and may require alternative treatments.

OSA Symptoms
The symptoms of each type of Sleep Apnoea overlap; common warning signs and symptoms include:
- Gasping or choking during sleep
- Loud snoring
- Breathing pauses during sleep
- Feeling excessively tired during the day
- Anxiety
- Depression
- High Blood Pressure
- Lack of interest in sex
- Irritability
- Short temper
- Poor memory and concentration
- Frequent toilet visits during the night
- Morning headaches
- Teeth grinding
- Impotence in men
You may also feel constantly tired and unable to sleep properly.
What causes Sleep Apnoea?
The causes of Sleep Apnoea, depends on the type and the individual. OSA is caused by an airway obstruction during sleep. Contributing factors include traits that can narrow the airway and hinder airflow such as large tonsils and obesity.
CSA is caused by disruptions that interfere with the brain’s control of breathing; these can include hormonal changes, medical conditions and certain medications.
Complex Sleep Apnoea also known as treatment emergent central apnoea has been found to occur in as little as 1.5% of people treated for OSA with CPAP therapy (2). It occurs when central apnoea episodes appear as a side effect of treatment, even though the obstructive events are resolved.
How is Sleep Apnoea diagnosed?
Sleep Apnoea is diagnosed via a sleep test, which can be conducted at home, a private sleep clinic or through the NHS.
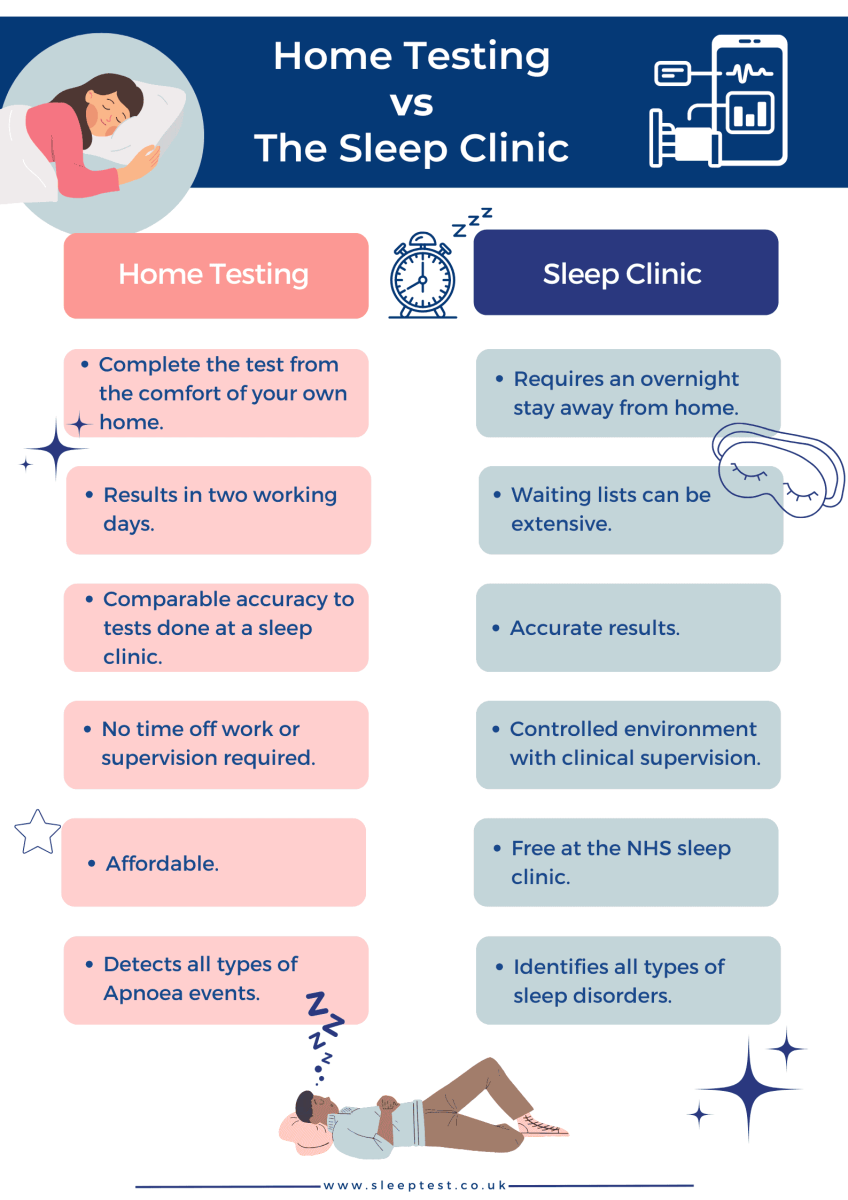
Home Sleep Tests vs Sleep Clinic
A private home sleep test is an effective alternative to going to your GP and visiting the sleep clinic if you have symptoms of Sleep Apnoea.
Many choose our private WatchPAT test because it provides results much quicker than going through the NHS sleep clinic.
The hassle-free test is delivered straight to your door, takes just one night to complete from home and results are with you within two working days.
Your results are confidential and only shared with you, plus the simple WatchPAT test is clinically validated and is frequently used in both NHS and private sleep clinics providing a high level of accuracy for diagnosing Obstructive Sleep Apnoea.
We also include a complimentary follow-up clinical consultation with NHS-trained sleep professionals if OSA is diagnosed.
How is Sleep Apnoea treated?
Sleep Apnoea treatment is necessary to control the symptoms so you can sleep better and reduce the risk of other health complications developing. Treatment is dependent on the type of Sleep Apnoea and the severity; the most common treatment types include:
CPAP Therapy: Continuous Positive Airway Pressure (CPAP) Therapy keeps the airway open by providing continuous airflow. The pressurised air is delivered through a CPAP machine via a tube and face mask. CPAP is classed as the gold-standard treatment as it provides effective results to millions of OSA sufferers around the world.
Mandibular Advancement: Mandibular Advancement Devices (MADs) are mouthguards that gently pull the tongue and lower jaw forward. This motion creates more space at the back of the throat to increase airflow and prevent airway blockages. MADs use a boil-and-bite method to create a customised and comfortable fit.
Positional Therapy: Positional therapy is designed for those diagnosed with positional sleep apnoea, where apnoea events occur exclusively or predominantly when sleeping on their back. This happens as the tongue and soft tissues of the throat drop back, causing a blockage of the airway. Positional therapy helps by encouraging the user to roll over onto their side to keep the airway open.
Lifestyle Changes: The majority of people with Sleep Apnoea will be asked to make changes in their day-to-day lives to help reduce their symptoms. These changes may include:
- Limiting alcohol consumption
- Quitting smoking
- Losing weight
- Creating a bedtime routine
- Practising relaxation techniques
- Clearing your sinuses
Learn more in our lifestyle adjustments for better sleep article.
Risks of untreated Sleep Apnoea?
Many wonder if OSA can cause them to choke to death or suffocate from repeated breathing pauses. It is unlikely for this to happen. However, when OSA is untreated, the risk of long term health conditions developing increases.
When the body’s oxygen levels repeatedly drop, it triggers the body to release stress hormones which increase your heart rate and blood pressure. This ongoing strain puts you at a higher risk of cardiovascular conditions, including:
- Heart attack
- Stroke
- Atrial Fibrillation
- Heart failure
- Heart disease
Other complications include:
- Eye problems: Some research suggest a connection between Obstructive Sleep Apnoea and certain eye conditions, such as glaucoma (3).
- Alzheimer’s: There is a potential link between untreated Sleep Apnoea and the development of Alzheimer’s due to cognitive decline and memory loss (4).
- Type 2 diabetes: The oxygen deprivation associated with the condition can worsen insulin resistance and lead to difficulty regulating blood sugar levels, increasing the risk of developing Type 2 diabetes.
Risk Factors
Age: It is more common in older adults as the muscles in the throat may weaken overtime, increasing the risk of airway blockages during sleep.
Body weight: Carrying extra weight, especially around your neck, can narrow the airway and make your throat muscles more likely to collapse during sleep.
Being male: Studies have found that men are more likely to develop Sleep Apnoea. A review of various studies found an average prevalence of 22% in males and 17% in females (1).
Smoking: Smoke irritates the throat and lungs, increasing the likelihood of airway blockages.
Family history: If someone in your family has Sleep Apnoea, you might be at a higher risk due to genetic factors.
Hormonal differences: Your hormone levels can impact muscle tone and airway function affecting your ability to breathe during sleep.
Congestion: Problems with nasal passages, such as allergies, frequent congestion, or a deviated septum, can make breathing through the nose harder.
Medications: Certain medications can relax the muscles and increase the risk of airway blockages during sleep, contributing to Sleep Apnoea.
Alcohol: Alcohol can relax the throat muscles, making them more likely to collapse during sleep.
Other medical conditions: Conditions such as diabetes, stroke, heart failure, high blood pressure and hormonal conditions can increase the risk.
The risk factors for OSA and CSA do overlap; however, some factors are directly linked to Central Sleep Apnoea:
Brainstem problems: Issues with the brainstem, which regulates breathing, can lead to CSA.
High altitude: Being at high altitudes with less oxygen in the air can temporarily trigger CSA, especially if you’re not used to it.
These factors can disrupt the brain’s signals to the muscles that control breathing during sleep, leading to episodes of interrupted breathing.
Summary
For over twenty years, we have helped thousands of people regain quality sleep and lead healthier lives with our reliable sleep testing and treatment options.
We are here every step of the way, from diagnosing OSA to starting and continuing treatment. If you have any questions about Sleep Apnoea, your symptoms or how to get tested, please contact us.
About Our Editorial Team
Danni is a degree-educated content writer passionate about helping those with Sleep Apnoea sleep better; she works closely with our clinical and customer care teams to ensure that each article is thoroughly researched and accurate.
Her writing aims to inform, support, and advise readers about Sleep Apnoea, helping to raise awareness and promote effective treatment options.
She has written many health-focused articles, reaching hundreds of readers annually, to help people sleep better and live healthier lives.
Lateisha King is an experienced Sleep Clinician with advanced training in polysomnography and respiratory health.
With over six years of experience, including at the prestigious Guy’s and St Thomas’ NHS Foundation Trust Hospital, she has conducted and reviewed more than 500 diagnostic sleep studies.
Her expertise in sleep science ensures that all articles align with the latest data and treatment protocols, providing readers with trustworthy and practical advice to improve their sleep health and overall well-being.
References
- Franklin KA, Lindberg E. (2015). Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4561280/. Accessed: 10.04.2024
- Javaheri S, Smith J, Chung E. The prevalence and natural history of complex sleep apnea. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC2699163/. Accessed: 20.01.2025.
- Sun C, Yang H, Hu Y, Qu Y, Hu Y, Sun Y, Ying Z, Song H. (2022). Association of sleep behaviour and pattern with the risk of glaucoma: a prospective cohort study in the UK Biobank. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9644340/. Accessed: 17.01.2025
- Bubu OM, Brannick M, Mortimer J, Umasabor-Bubu O, Sebastião YV, Wen Y, Schwartz S, Borenstein AR, Wu Y, Morgan D, Anderson WM. (2017). Sleep, Cognitive impairment, and Alzheimer’s disease: A Systematic Review and Meta-Analysis. Available at: https://pubmed.ncbi.nlm.nih.gov/28364458/. Accessed: 17.01.2025






